Muscle contusions are prevalent injuries in sports, often resulting in significant morbidity (morbidity is the state of being symptomatic or unhealthy due to a disease or condition) among athletes. Understanding the presentation, physical examination, diagnostic testing, treatment, and potential complications of these injuries is crucial for effective management and optimal outcomes.
Muscle contusions are also second only to strains in sports-related injuries, and they vary in severity depending on factors such as:
- Impact site
- Muscle activation status
- Patient age
- Fatigue presence.
Quadriceps strains and contusions are particularly common, leading to training and competition downtime. While management acronyms like ICE, RICE, PRICE, and POLICE have guided acute care, attention to subacute and chronic healing stages is essential. Additionally, acronyms such as PEACE and LOVE have been proposed for optimal management.
Differentiating between Muscle Contusions and Hematomas
Muscular hematomas and muscular contusions are typically manageable conservatively, involving bleeding within muscle groups.
A contusion, also known as a bruise, typically appears on the skin after trauma such as a blow to the body. It occurs when the small veins and capillaries under the skin break. A hematoma, on the other hand, is a collection (or pooling) of blood outside the blood vessel.
While clinical judgment has traditionally sufficed for diagnosis, newer modalities like ultrasonography and MRI are increasingly crucial for identifying and delineating injuries. Understanding the natural healing process, including muscle repair, regeneration, and scar tissue formation, aids in tailored management.
Physical Examination
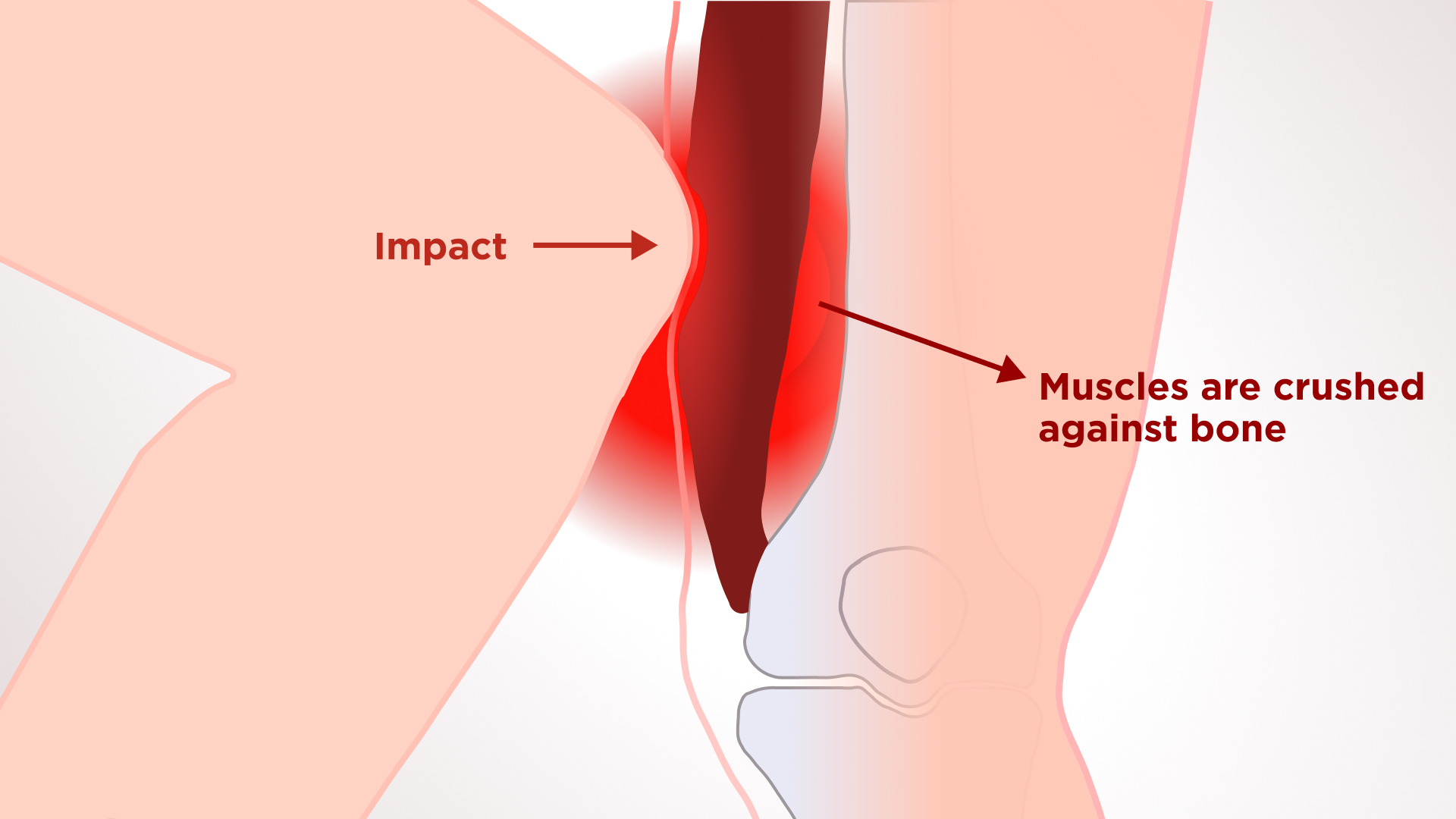
Perhaps more so than with muscle strains, athletes will usually report a definite mechanism associated with a contusion injury. A direct blow from an opponent’s knee or other piece of equipment is frequently recalled as the traumatic force causing their pain. Localized pain at the site of injury, swelling, decreased range of motion, and tenderness to palpation are usual findings. Ecchymosis may not develop until 24 hours after the injury. Depending on the severity of the injury, some athletes may be able to continue their activity and present after competition or training for evaluation.
Upon examination, the area of injury should be inspected for obvious deformity, swelling, or ecchymosis. Palpation along the injured muscle will help localize the exact site of muscle damage and determine if there is any associated injury. Strength testing of the muscle, for example, if the quadriceps muscle is injured, will be performed by resisting knee extension and hip flexion. Comparing the uninjured side will aid in assessing the severity of the injury.
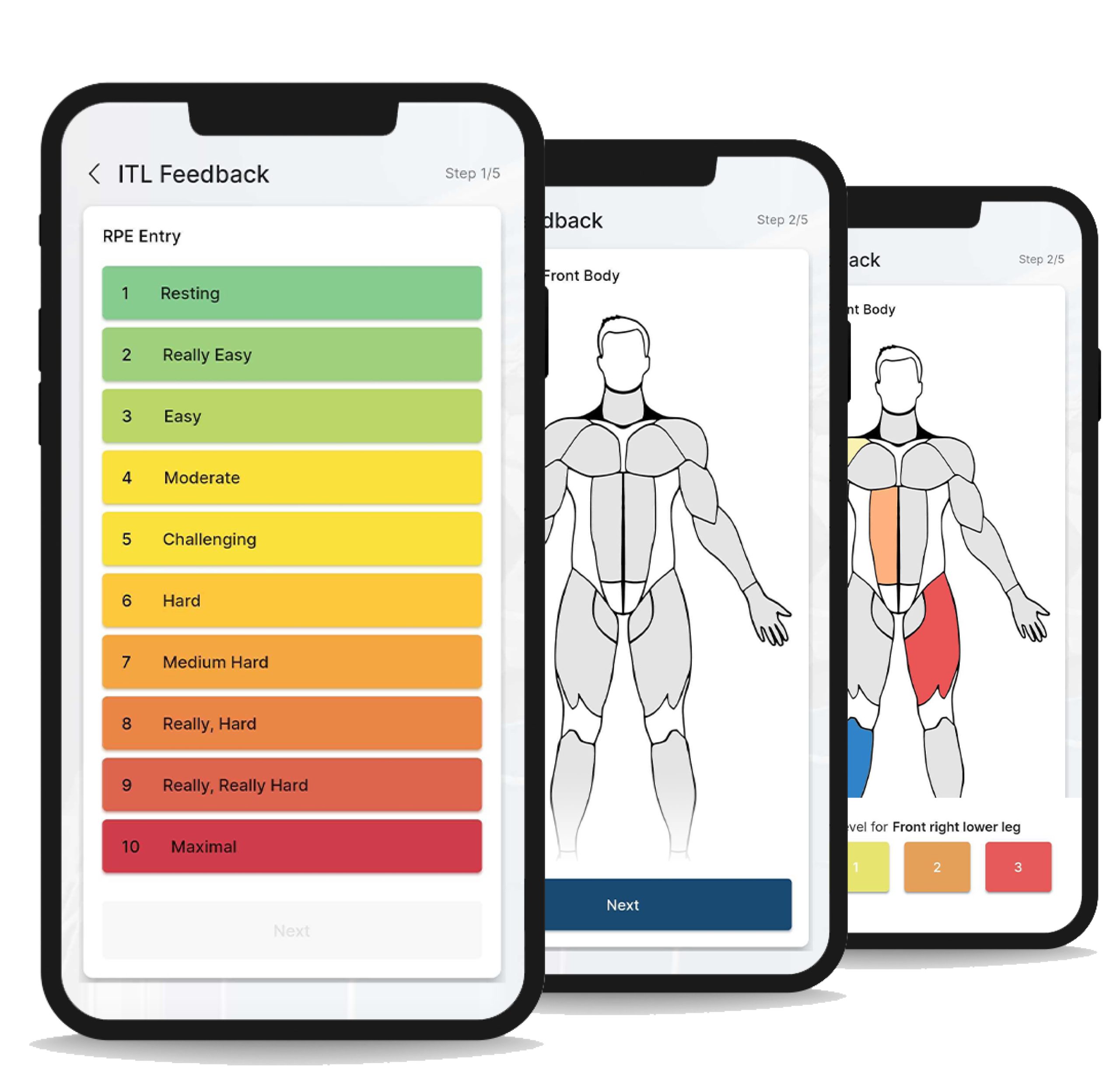
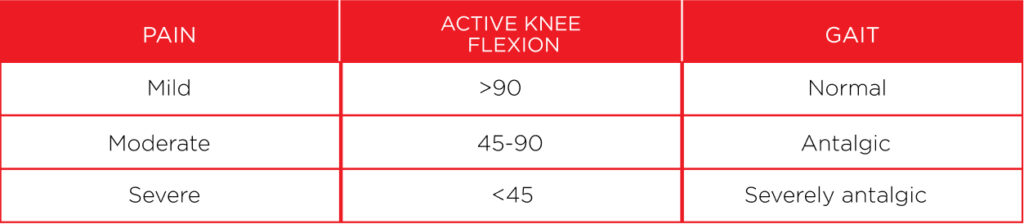
Measurement of knee flexion has been used as a prognostic indicator in quadriceps contusions. Jackson and Feagin originally described a classification system (Table 1), which was further modified by Ryan et al. Mild contusions are characterized by a normal gait, localized tenderness, and active knee flexion of greater than 90 degrees. Moderate contusions are characterized by an antalgic gait, swollen, tender mass in the quadriceps, and 45–90 degrees of active knee flexion. Severe contusions are characterized by a severely antalgic gait, noticeably swollen and tender muscle mass.
Imaging
While most acute quadriceps injuries can be diagnosed clinically, imaging aids in uncertain cases or when detailed injury characterization is necessary. Radiographs, ultrasound, and MRI offer valuable insights into muscle and tendon injuries, guiding treatment planning.
Radiographs are routinely normal in acute muscle strains but may be helpful in differentiating between bony (femoral stress fracture, tumor, or myositis ossificans) and muscular etiologies of quadriceps pain in chronic cases.
Ultrasound is an excellent imaging modality for visualizing the quadriceps muscles and tendons, but it is highly operator-dependent and requires a skilled and experienced clinician. Ultrasound has the ability to image the muscles dynamically and assess bleeding and hematoma formation via Doppler.
MRI provides detailed images of muscle injury and can be quite helpful in characterizing quadriceps injuries. However, it can sometimes be difficult to distinguish between muscular contusion and strain on MRI, which reinforces the importance of clinical history and examination in injury assessment.
Treatment: Chronic and Acute Care
Studies are being performed to evaluate the effects of anti-inflammatory medications, corticosteroids, operative repair, and exercise protocols. However, treatment of muscle contusion injuries has not changed greatly over the years, and there is little scientific basis for the majority of treatment protocols.
Treatment principles focus on minimizing bleeding, inflammation, and promoting optimal tissue repair. Early intervention by PEACE and LOVE principles emphasizes protection, elevation, avoiding anti-inflammatory modalities, compression, education, loading, optimism, vascularization, and exercise.
We have to keep in mind that anything that reduces inflammation also delays healing since the process of inflammation is an essential aspect of recovery itself.
Although cold therapy typically slows soft tissue swelling to some extent, it does not hasten the recovery process. Ice could be a useful option when our treatment goal is to limit the extent of edema, since excessive or prolonged swelling has been proven to impede the healing process, particularly in severe joint sprains. However, when the edema level is not severe (e.g., muscle tear), cold therapy may not be helpful and could instead act as a barrier to recovery.
Compression may help decrease blood flow, and when accompanied by elevation, it will serve to decrease both blood flow and excess interstitial fluid accumulation.
While anti-inflammatories show benefits in pain management and function improvement, our acronyms flag their potential harmful effects on optimal tissue repair.
PEACE
P for Protect
Unload or restrict movement for 1–3 days to minimize bleeding, prevent distension of injured fibers, and reduce the risk of aggravating the injury. However, rest should be minimized, as prolonged rest can compromise tissue strength and quality. Pain signals should guide the cessation of protection.
E for Elevate
Elevate the limb higher than the heart to promote the flow of interstitial fluid out of tissues. Despite weak evidence supporting its use, elevation demonstrates a low risk-to-benefit ratio.
A for Avoid Anti-inflammatory Modalities
The various phases of inflammation play a crucial role in repairing damaged soft tissues. Thus, inhibiting inflammation using medications may negatively affect long-term tissue healing, especially when higher dosages are used. NSAIDs inhibit cyclooxygenase (COX) enzymes in the arachidonic acid (ArA) pathway to reduce the synthesis of prostaglandins. Therefore, the standard of care for soft-tissue injuries should not include anti-inflammatory medications.
We also question the use of cryotherapy. Despite widespread use among clinicians and the population, there is no high-quality evidence on the efficacy of ice for treating soft-tissue injuries. Even though it may provide some analgesic relief, ice could potentially disrupt inflammation, angiogenesis, and revascularization, delay neutrophil and macrophage infiltration, and increase immature myofibers. This could lead to impaired tissue repair and redundant collagen synthesis.
C for Compress
External mechanical pressure using taping or bandages helps limit intra-articular edema and tissue hemorrhage. Despite conflicting studies, compression after an ankle sprain appears to reduce swelling and improve quality of life.
E for Educate
Therapists should educate patients on the benefits of taking an active approach to recovery. Passive modalities, such as electrotherapy, manual therapy, or acupuncture, used early after injury, have insignificant effects on pain and function compared to an active approach and may even be counterproductive in the long term. Indeed, fostering an external locus of control or the belief that one needs to be fixed can lead to therapy-dependent behavior.
Better education on the condition and load management will help avoid overtreatment, which in turn reduces the likelihood of unnecessary injections or surgery and supports a reduction in healthcare costs (e.g., disability compensation associated with low back pain). In an era of high-tech therapeutic options, we strongly advocate for setting realistic expectations with patients about recovery times instead of chasing the ‘magic cure’ approach.

LOVE
L for Load
An active approach involving movement and exercise is beneficial for most patients with musculoskeletal disorders. Mechanical stress should be introduced early, and normal activities should be resumed as soon as symptoms allow. Optimal loading without exacerbating pain promotes repair, remodeling, and builds tissue tolerance and the capacity of tendons, muscles, and ligaments through mechanotransduction.
O for Optimism
Optimistic patient expectations are associated with better outcomes and prognosis. However, psychological factors such as catastrophization, depression, and fear can represent barriers to recovery. Beliefs and emotions are thought to explain more of the variation in symptoms following an ankle sprain than the degree of pathophysiology.
V for Vascularization
Cardiovascular activity plays a crucial role in the management of musculoskeletal injuries. While more research is needed on dosage, pain-free aerobic exercise should be initiated a few days after injury to boost motivation and increase blood flow to the injured structures. Early mobilization and aerobic exercise improve physical function, support return to work, and reduce the need for pain medication in individuals with musculoskeletal conditions.
E for Exercise
There is strong evidence supporting the use of exercise for the treatment of ankle sprains and for reducing the prevalence of recurrent injuries. Exercises aid in restoring mobility, strength, and proprioception early after injury. Pain should be avoided to ensure optimal repair during the subacute phase of recovery and should serve as a guide for exercise progressions.
Managing soft-tissue injuries involves more than short-term damage control. All strengthening exercises should be performed through a pain-free range of motion. Advancement through each type of strengthening depends on the level of soreness and pain created by each exercise. For example, once isometric straight leg raises at 0, 20, and 40 degrees can be completed without any pain or subsequent soreness, isotonics can then be initiated.
Maintaining aerobic fitness during rehabilitation can be accomplished by using activities like swimming and biking.
Complications: Myositis Ossificans and Compartment Syndrome
Complications of muscle contusions can include the formation of large hematomas, which can lead to increased morbidity and extended healing time. One potential complication is myositis ossificans (MO), where bone or bone-like tissue forms in areas where it shouldn’t. This condition often occurs in muscles following significant trauma, such as a hard impact to the thigh during sports or accidents, and it’s estimated to occur in up to 20% of cases involving large hematomas. Typically, about 80% of these bony growths develop in the muscles of the thigh or upper arm.
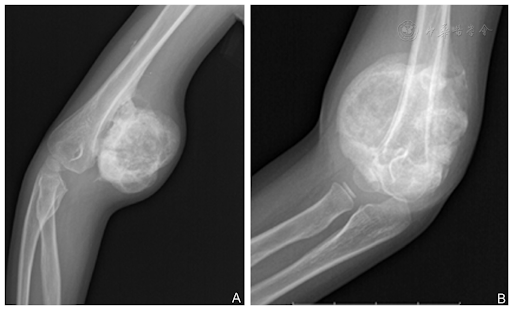
Most contusions, strains, and hematomas tend to improve after a few days or weeks with therapy. However, with myositis ossificans (MO), the pain tends to worsen, and the range of motion in the affected limb typically decreases within one to two weeks after the initial injury. Symptoms of MO include progressive pain, swelling, and loss of range of motion in the affected muscle group. Patients may also notice palpable nodules or areas of induration within the muscle tissue. Initially, the symptoms of myositis ossificans can resemble those of a severe muscle contusion, which can make early diagnosis challenging.
Characteristic findings of ossification within the muscle tissue may be revealed by X-ray, while ultrasound and MRI offer detailed visualization of the extent and location of ectopic bone formation.
If myositis ossificans has already been diagnosed, treatment typically follows a conservative approach similar to the initial injury management. Physical therapy is often recommended, as symptoms tend to improve over time, and the size of the bony mass may decrease.
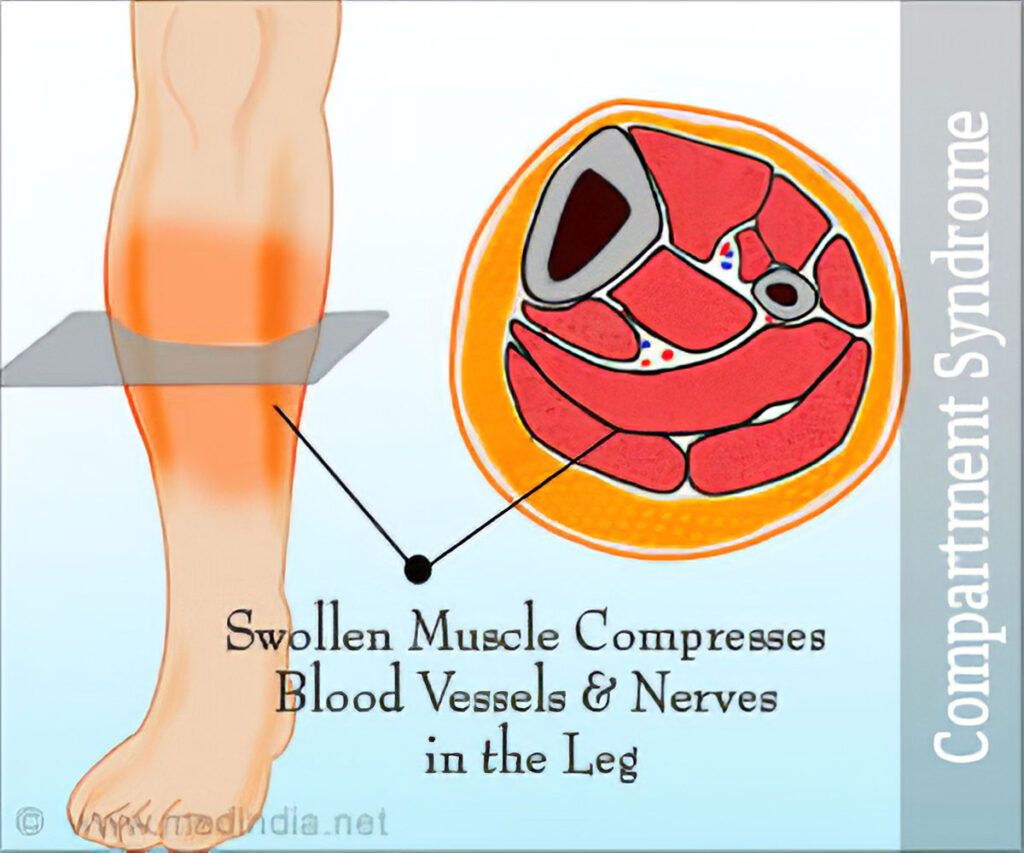
Compartment Syndrome: A Threat to Limb Viability
Compartment syndrome is a serious condition characterized by increased pressure within a closed muscle compartment, resulting in impaired tissue perfusion and potential tissue necrosis. While rare, it can occur as a result of traumatic muscle injuries such as contusions, and prompt recognition and intervention are essential to prevent long-term complications. Although there are some reports of compartment syndrome appearing as late as 8 days after injury, symptoms typically onset within the first 24 hours following the injury.
Compartment syndrome typically arises following a significant increase in intracompartmental pressure. Elevated pressure within the muscle compartment impairs tissue perfusion, leading to ischemia and potentially irreversible tissue damage if left untreated.
Patients with compartment syndrome may present with severe pain, swelling, and tenderness in the affected limb, which may be disproportionate to the degree of injury. Pain can be exacerbated by passive stretching of the involved muscles, and sensory deficits or motor weakness may also be present. In severe cases, patients may exhibit signs of neurovascular compromise, such as pallor, pulselessness, or paralysis.
The diagnosis of compartment syndrome is primarily clinical, based on a thorough history and physical examination.
Treatment involves emergent surgical decompression of the affected compartment to relieve pressure and restore tissue perfusion. Fasciotomy, the surgical release of the affected compartment’s fascia, is the definitive treatment for compartment syndrome.
Conclusion
In conclusion, muscular contusions rank as the second most common cause for absence from training and matches. Therefore, it’s crucial to minimize the days players spend absent from normal training and set realistic expectations regarding injury management time. Utilizing the PEACE and LOVE principles as a guide in treatment can aid in effective recovery.
To prevent complications, it’s essential to remain vigilant, treat injuries accordingly, and be prepared in case complications do arise. By proactively addressing potential issues and adhering to proper treatment protocols, the likelihood of complications can be minimized, ultimately promoting better outcomes for athletes.
References
- Dubois, B., & Esculier, J. F. (2020). Soft-tissue injuries simply need PEACE and LOVE. British Journal of Sports Medicine, 54(2), 72-73. doi: 10.1136/bjsports-2019-101253. PMID: 31377722.
- Hoth, P., & Amendola, A. (2014). Contusions, Myositis Ossificans, and Compartment Syndrome of the Thigh. DOI:10.1007/978-1-4899-7510-2_9
- Kary, J. M. (2010). Diagnosis and management of quadriceps strains and contusions. Current Reviews in Musculoskeletal Medicine, 3(1-4), 26-31. doi: 10.1007/s12178-010-9064-5. PMID: 21063497; PMCID: PMC2941577.
- https://motusspt.com/compartment-syndrome/